Gastroscopy
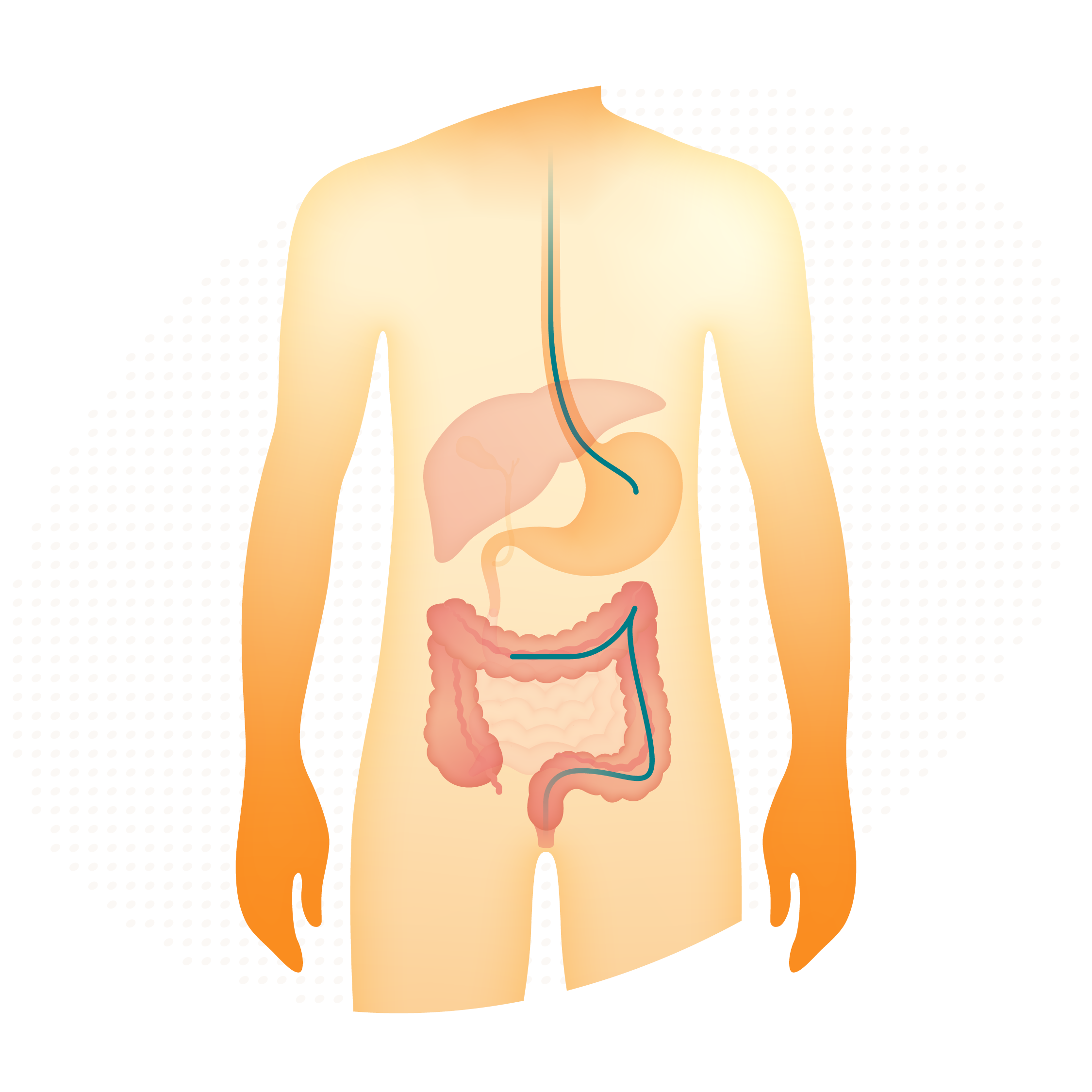
A gastroscopy uses a thin, flexible tube to examine your oesophagus, stomach and duodenum. This procedure is used to check the health of your gut when you have the following symptoms:
- Upper abdominal pain
- Heartburn not responsive to medication
- Difficulty swallowing
- Vomiting, especially blood
- Persistent nausea and vomiting
- Black, tar-like bowel motions
- Unexplained weight loss
Typical pathologies found include oesophagitis, hiatal hernias, ulcers or digestive conditions such as coeliac disease.
Colonoscopy
A colonoscopy involves using a slim, flexible tube with a small camera on the end to look inside your bowel. This is used to check the health of your bowel when you have the following symptoms:
- Blood loss from the bowel (aka rectal bleeding).
- A change of bowel habit, such as ongoing diarrhoea.
- Low abdominal pain that may suggest inflammation of the colon.
- To check for polyps.
- To re-examine the colon after a polyp, or cancer, has been removed and to check that no new growths have developed.
- To check those who have a family history of bowel cancer or a genetic condition that predisposes them to cancer.
Colonoscopy and gastroscopy
Click the sections below to watch videos and learn more about each surgery.

What to expect
- During your consultation We’ll review your medical history together and discuss the symptoms you’re having to help me determine the severity of the situation and determine the best course of action.
- After your consultation We’ll book you in for your procedure and provide detailed pre-op information and instructions to make sure you fully understand what to expect on the day of the procedure, including a detailed outline of your planned post-op care.
Colonoscopy, a pre-op and post-op guide
Bowel preparation dose and method of administration
It is essential that the bowel is clean prior to colonoscopy. Bowel preparation requires two sachets of Picosalyx taken several hours apart, starting the day before the procedure. The timing of these two sachets depends on what time of the day your colonoscopy is booked. Each sachet is mixed with 150 mL (2/3rds of a cup) of water and stirred for 2 to 3 minutes so it becomes an off-white, cloudy liquid with a faint odour of orange. If it becomes warm, wait until it cools sufficiently to drink. Drink the solution. Do not prepare the solution in advance.
Note that:
The sachet must be taken the afternoon of the day before if the procedure is planned before 1pm.
The sachet must be taken the night before if the procedure is scheduled after 1pm.
For more information about the preparation, download the colonoscopy guide below.
What happens in a colonoscopy?
Most colonoscopies are performed at Southern Endoscopy Centre but occasionally at St Georges Hospital or Southern Cross Hospital. Colonoscopies are performed as a day-case procedure, so you will need someone to drop you off and drive you home. Once admitted, you will be taken to the pre-op ward and asked to change into a gown. An IV will be placed in your arm so you can receive fluids and medication to help you relax and keep you comfortable during the procedure. When ready, you will be transferred to the endoscopy suite, where you’ll be asked to lie on a bed so that the nurses can attach monitors. The procedure is performed with you lying on your left side, knees curled up to your chest. As the colonoscope is inserted, it is not unusual to feel pressure, cramping and the feeling of needing to evacuate. This is because of the gas used to distend the colon for a better view. The aim is to advance the colonoscope to the end of the colon and then slowly withdraw to look for things like polyps or masses; if found, they may be removed or biopsied. The whole procedure takes around 30 minutes. Afterward, you’ll spend some time in recovery while the sedation wears off. You will be given food and drink when you recover alertness. You may feel a bit gassy or have mild cramping, but this usually settles quickly. You’ll need someone to drive you home, and you can usually get back to normal activities the next day, though you should take it easy for the rest of the day.
Will I be awake?
Most colonoscopies are performed under sedation, meaning you are not unconscious. Intravenous drugs are given to induce relaxation and control discomfort. Usually patients describe a drowsy feeling that quickly turns into a light sleep, though they can be roused if necessary.
For more information, download the colonoscopy guide below.
Resting time
You should take it easy for the rest of the day, as the sedation can make you drowsy and affect your coordination and judgement. For 24 hours following the procedure, you should not:
drive.
operate heavy or potentially harmful machinery.
make legally binding decisions.
Hydrate
Drink plenty of liquids to help your body recover. You no longer need to restrict yourself to clear fluids, but it is advisable to avoid alcohol for 24 hours.
Eat light
Start with light, easily digestible foods such as toast, crackers, bananas, etc. Avoid heavy, greasy foods for 24 hours.
Passing gas
Bloating, mild discomfort and flatulence are common following the procedure. Walking, warm liquids, and heat packs to the abdomen can help relieve these.
Medications
Take your medications exactly as prescribed on your medication discharge instruction sheet. Unless otherwise directed by your doctor, all of your medications and vitamins can be swallowed as they are given. Alternatively, you may crush tablets or use chewable or liquid forms.
For more information about your medication, download the colonoscopy guide below.
Gastroscopy, a pre-op and post-op guide
Before the procedure
Fasting: Do not eat any food for at least 6 hours before your gastroscopy. Your stomach must be empty for the procedure to be safe and accurate. You may be allowed small sips of water up to 2 hours before your appointment, but check your specific instructions.
Medications: Most regular medications can be taken with a small sip of water. However, some medications may need to be stopped or adjusted (see medications in the post-op section below).
Smoking and gum: Do not smoke or chew gum on the day of your procedure, as these can increase stomach secretions and affect your results.
The day of your gastroscopy
Arrive at the hospital or clinic 10 minutes before your scheduled time. Wear loose, comfortable clothing and leave valuables at home.
Bring your referral if you have it, your list of medications, and any forms provided by your doctor.
If you are having sedation, you must arrange for an adult to collect you after the procedure.
For more information, download the gastroscopy guide below.
What happens in a gastroscopy
Most gastroscopies are performed at Southern Endoscopy Centre but occasionally at St Georges Hospital or Southern Cross Hospital. Gastroscopies are performed as a day-case procedure, so you will need someone to drop you off and drive you home.
Once admitted, you will be taken to the pre-op ward and may be asked to change into a gown. An IV will be placed in your arm so you can receive fluids and medication to help you relax and keep you comfortable during the procedure.
When ready, you will be transferred to the endoscopy suite, where you’ll be asked to lie on a bed so that the nurses can attach monitors. The procedure is performed with you lying on your left side. An anaesthetic mouth spray is given to stop any gag reflex. You will be asked to bite onto a mouth guard that will be tied into position. This ensures you don’t inadvertently bite through the scope.
Once the sedation takes effect, the gastroscope is inserted through the mouth and advances as far as the duodenum. It is common to feel a gassy, bloated feeling in the abdomen. This is because of the gas used to distend the stomach for a better view. The whole procedure takes around 10 minutes.
Afterward, you’ll spend some time in recovery while the sedation wears off. You will be given food and drink when the mouth spray wears off and you recover alertness. You may feel a bit gassy or have mild cramping, but this usually settles quickly.
You’ll need someone to drive you home, and you can usually get back to normal activities the next day, though you should take it easy for the rest of the day.
Rest
You should take it easy for the rest of the day, as the sedation can make you drowsy and affect your coordination and judgement. For 24 hours following the procedure, you should not:
drive.
operate heavy or potentially harmful machinery.
make legally binding decisions.
Hydrate
Drink plenty of fluids to help your body recover.
Eat light
Start with light, easily digestible foods such as toast, crackers, bananas, etc. Avoid heavy, greasy, or spicy foods for 24 hours.
Following the procedure
Mild discomfort and abdominal cramping may occur for a few hours after the gastroscopy. This is due to the gas used in the procedure. Walking, warm liquids, and heat packs to the abdomen can help relieve these. A sore throat is not uncommon for two days after the procedure. This is due to the tube passing through to your oesophagus. Ice chips, warm drinks, and Difflam lozenges can usually help relieve these.
Medications
Take your medications exactly as prescribed on your medication discharge instruction sheet. Unless otherwise directed by your doctor, all of your medications and vitamins can be swallowed as they are given. Alternatively, you may crush tablets or use chewable or liquid forms.
For more information about medications, get in touch or download the gastroscopy guide below.
Patient information for colonoscopy and gastroscopy procedures
Download our pre- and post-op patient guides for more information on what to expect during the process. Please note, these are general information brochures. When you are booked in for your procedure, you’ll receive any personalised information and details about your specific situation.

If you have unusual abdominal or bowel pain, I may be able to help.
Ask your GP to refer you to Richard Flint or get in touch with me to discuss your options.
FAQs
I am an independent surgeon, but I operate out of St George’s Hospital, one of Christchurch’s leading healthcare facilities. Enjoy comfortable surroundings and the support of dedicated nursing staff delivering quality care throughout your stay.
Gastroscopy or colonoscopy procedures rarely involve an overnight stay.
It depends on the type of medication. Here is a pre-op guide to find out more. If you have any doubt or further questions, don't hesitate to reach out to me or your GP.
The costs differ for each procedure. Here is a list of indicative costs for each of these procedures:
Endoscopy (the range depends on what is done)
Gastroscopy $2,861-$3,500
Colonoscopy $3,280-$4,040
Gastroscopy and colonoscopy combined $4,729-$5,464
Note that these prices are indicative.
Visit the FAQs if you have more questions, or get in touch with me for any other concerns.